Identifying Peripheral Neuropathy in Fall Patients with the Heat-Washout Method
Le Gjerum & Mette Midttun*
Introduction
Fall is a common problem among the elderly. About 1/3 fall every year from the age above 65 years, fall-related injuries increase with age, and furthermore, fall increases the risk of being admitted to a nursing home threefold1–4.
The prevalence of peripheral neuropathy among the 60 to 74 years old is estimated to 20% with the majority caused by diabetes mellitus, and the prevalence of both peripheral neuropathy and diabetes mellitus increases with age5-8. Additionally, diabetic patients with peripheral neuropathy have a fivefold increased risk of falling9–13.
In Denmark the patients, especially the elderly, who fall can be referred to the fall clinic, a specialized geriatric clinic, to identify and treat risk factors for falling, including screening for peripheral neuropathy with the monofilament and the tuning fork.
The potential increase in fall risk due to peripheral polyneuropathy may be a result of both large fibre and small fibre dysfunction. The symptoms of large fibre neuropathy mainly affect light touch, vibration sense, and proprioception possibly causing impaired balance, gait and muscle weakness, whereas the small fibre dysfunction can result in abnormal pain and temperature sensation causing impaired balance, and autonomic deficit causing postural hypotension14–17.
One of the clinical features of distal sympathetic small fibre neuropathy is orthostatic hypotension, which is a common symptom in the elderly and associated with increased fall risk18–20.
The veno-arteriolar reflex is a local cutaneous reflex in the peripheral autonomic nervous system, associated with postural changes and orthostatic hypotension21,22. Previous studies indicate that the veno-arteriolar reflex is impaired in type 2 diabetics with neuropathy, when estimated with the laser Doppler flowmetry and the heat-washout method23–26.
It is essential to diagnose peripheral neuropathy as it is often associated with treatable systemic disorders, furthermore, early identification of peripheral neuropathy may be an important element in preventing falls, but the clinical evaluation of peripheral neuropathy in the elderly can be very challenging27,28, among others because the cognitively impaired patients may have difficulties understanding and responding verbally to the examination tests, and thus indicating if the perception is perceived. Furthermore, the common symptoms of peripheral neuropathy may not be as straightforward in older patients6,8.
The most commonly used, routine clinical diagnostic tools for assessing peripheral nerve dysfunction in diabetic patients and fall patients are examination of vibration perception threshold with the tuning fork, and sensory perception with the monofilament, while the vibration perception threshold measured by the biothesiometer is often used as a gold standard for peripheral neuropathy5,11,15,29–33. The validation of these tests is, however, challenged by a number of factors related to both the patient and the clinician, furthermore, they are only useable for assessing large fibre neuropathy5,15,34.
The evaluation of the orthostatic blood pressure is fairly straightforward and is readily done in clinical practice as part of the fall assessment32.
The aim of this present study was to evaluate the routine clinical modalities for examine peripheral neuropathy in the geriatrician fall assessment, and to compare these methods to an objective method, the heat-washout method, which may be a better option when assessing peripheral neuropathy in older, fall patients:
• Examine elderly fall patients diagnosed with peripheral neuropathy with the heat-washout method for assessing the veno-arteriolar reflex.
• Compare the results from the heat-washout method with three commonly used simple neurological screening methods:
• The monofilament for assessing loss of protective sensation.
• The tuning fork for assessing impaired vibratory sensation.
• The biothesiometer for assessing impaired vibratory sensation.
• Compare the result from the heat-washout method with the orthostatic blood pressure for assessing the peripheral autonomic nervous system.
Methods
Fifteen patients diagnosed with peripheral neuropathy according to the ICD10 codes35 in relation to the fall assessment were enrolled in the study in the Fall clinic at department of Internal Medicine, Geriatric section at Copenhagen University Hospital, Herlev, Denmark. The patients were diagnosed with peripheral neuropathy by medical doctors in the fall clinic based on the patient's clinical history, examination, and diagnostic assessment with the routine clinical bedside tests in the fall assessment: The monofilament and the tuning fork.
Mean age was 76.2 years (range 62-86 years), 7 males, and 8 females. One patient was diagnosed with type 2 diabetes and treated with Insulin.
All patients included in this study were tested for peripheral neuropathy with the monofilament, the biothesiometer, the tuning fork, and the heat-washout method in the Fall clinic. Additionally, all the patients were tested with orthostatic blood pressure corresponding to the fall assessment. Generally, the examination with the monofilament and the tuning fork were achieved in relation to standardized clinical evaluation according to the visit at the Fall clinic. The other tests, including any absent above-mentioned neurologic test, were performed at a second visit in the Fall clinic by a clinician.
The study protocol was approved by the Ethical Committee (H-15002239), and the Danish Health and Medicines Authority. All the participants provided written informed consent.
The biothesiometer, the tuning fork, the monofilament, and the orthostatic blood pressure:
The biothesiometer: Vibration perception threshold was measured with the biothesiometer. The probe was bilaterally applied perpendicularly to the apex of hallux. The voltage was gradually increased by the clinician, and vibration perception threshold was defined as the voltage level, when the patient first felt the vibration. The test was repeated three times on each foot, and a mean was taken. A mean vibration perception threshold value equal to or above 25 mV was considered abnormal, and an indication of peripheral neuropathy30,33.
The tuning fork: The vibration perception was, furthermore, tested with the 128 Hz tuning fork. The tuning fork was applied bilaterally with the on-off method to the medial malleolus. Absent or reduced perception on either malleolus was considered abnormal, and an indication of peripheral neuropathy36.
The monofilament: The pressure perception was examined with the monofilament. The monofilament was applied bilaterally on the sole of the foot on three standard points (plantar surface of distal hallux, 1st and 5th metatarsal heads).
The patient was prevented from seeing when and where the clinician applied the monofilament. The patient was instructed to indicate, when the perception of the monofilament was recognised, and subsequently identify on which foot the perception was perceived. Inability to perceive the sensation at any sites was considered abnormal and an indication of peripheral neuropathy37.
The orthostatic blood pressure: The patient's blood pressure was measured initially with the patient in supine position, afterwards the patient was changing position from supine to up-right posture and blood pressure was measured immediately and every minute for at least five minutes. A reduction of systolic blood pressure of at least 20 mm Hg or diastolic blood pressure of at least 10 mm Hg within 3 minutes of standing was considered abnormal and an indication of orthostatic hypotension38,39.
The heat-washout method:
The heat-washout method is an objective, non-invasive method measuring the blood flow rate in ml (100 g . min)-1 in the 2-3 mm superficial layer of the skin (the cutis) to examine the presence of the veno-arteriolar reflex, a cutaneous sympathicus reflex. The patient was covered with blankets during the examination to ensure warm hands and feet and thus dilated arterioles to achieve a maximal cutaneous blood flow rate.
The probe was attached on the skin in the first toe interstice of the forefoot avoiding visible veins. The foot was placed at heart level during the first measurement, and 50 cm below heart level at the second measurement, resulting in an increase in the toe blood pressure of approximately 40 mm Hg. A reduction in the blood flow rate of more than 30% with the foot placed below heart level indicated that the veno-arteriolar reflex was present. Lack of the veno-arteriolar reflex indicates that the peripheral sympathetic nervous system may be damaged due to neuropathy26. For detailed information of the heat-washout method, please see Midttun et al. 2013 and 199626,40.
All the patients tolerated the heat-washout method without any discomfort.
Results
We found that eleven of the fifteen patients had impaired veno-arteriolar reflex in both legs. In three patients the veno-arteriolar reflex was only impaired in one leg (table 1).
| Table 1. The observations in patients with peripheral neuropathy. | ||||||
| No: | Foot: | Monofilament: | Tuning fork: | Biothesiometer: | Heat-washout method: | Orthostatic Blood Pressure: |
|---|---|---|---|---|---|---|
| 1 |
Right: Left: |
Normal Normal |
Abnormal Abnormal |
Normal Abnormal |
Normal Normal |
Normal |
| 2 |
Right: Left: |
Normal Normal |
Abnormal Abnormal |
Normal Normal |
Abnormal Abnormal |
Abnormal |
| 3 |
Right: Left: |
Normal Normal |
Abnormal Abnormal |
Abnormal Normal |
Normal Abnormal |
Abnormal |
| 4 |
Right: Left: |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal |
| 5 |
Right: Left: |
Abnormal Abnormal |
Abnormal Abnormal |
Normal Normal |
Abnormal Abnormal |
Normal |
| 6 |
Right: Left: |
Normal Normal |
Abnormal Abnormal |
Normal Normal |
Abnormal Abnormal |
Normal |
| 7 |
Right: Left: |
Abnormal Abnormal |
Abnormal Normal |
Normal Normal |
Abnormal Abnormal |
Abnormal |
| 8 |
Right: Left: |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Normal Abnormal |
Normal |
| 9 |
Right: Left: |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Normal |
| 10 |
Right: Left: |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Normal Abnormal |
Abnormal |
| 11 |
Right: Left: |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Normal |
| 12 |
Right: Left: |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Normal |
| 13 |
Right: Left: |
Abnormal Abnormal |
Normal Abnormal |
Normal Abnormal |
Abnormal Abnormal |
Abnormal |
| 14 |
Right: Left: |
Normal Normal |
Normal Abnormal |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal |
| 15 |
Right: Left: |
Abnormal Abnormal |
Abnormal Abnormal |
Abnormal Normal |
Abnormal Abnormal |
Abnormal |
The result of the heat-washout method was consistent with the results of the biothesiometer in 50%, with the tuning fork in 73%, and with the monofilament in 70% (figure 1-3).
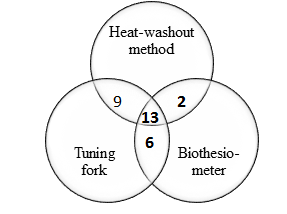
Figure 1:Venn diagram showing overlap between results for the heat-washout method, the tuning fork, and the biothesiometer. The heat-washout method overlapped with the tuning fork in nine cases and with the biothesiometer in two cases, overlap between the biothesiometer and the tuning fork in six cases. All three methods overlapped in thirteen cases.
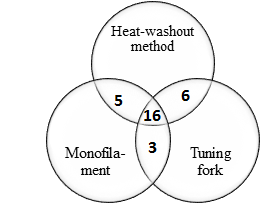
Figure 2:Venn diagram showing overlap between results for the Heat-washout method, the monofilament, and the tuning fork. The heat-washout method overlapped with the monofilament in five cases, and with the tuning fork in six cases, overlap between the monofilament and the tuning fork in three cases. All three methods overlapped in sixteen cases.
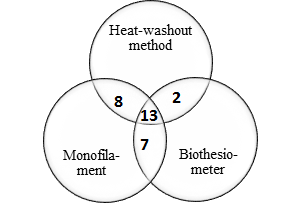
Figure 3:Venn diagram showing overlap between results for the heat-washout method, the monofilament, and the biothesiometer. The heat-washout method overlapped with the monofilament in eight cases, and with the biothesiometer in two cases, overlap between the monofilament and the biothesiometer in seven cases. All three methods overlapped in thirteen cases.
The result of the monofilament was consistent with the result of the tuning fork in 63%, and with the biothesiometer in 67%. The tuning fork and the biothesiometer correspondingly evaluated the vibrotactile perception, but there were only similar results in 63% (figure 4).
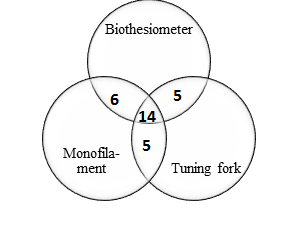
Figure 4:Venn diagram showing overlap between results for the biothesiometer, the monofilament, and the tuning fork. The biothesiometer overlapped with the monofilament in six cases, and with the tuning fork in five cases, overlap between the monofilament and the tuning fork in five cases. All three methods overlapped in fourteen cases.
We observed a similarity in the results between the heat-washout method and at least two of the three methods in 60% of the cases. We found full consistency between all four tests in 40% of the cases. In 47% we found full consistency between the monofilament, the tuning fork, and the biothesiometer.
We only observed disagreements between the results for the heat-washout method and the three other tests in 7% of the cases.
All the patients had abnormal results in at least one of the tests, with 90% abnormal result in the tuning fork, 67% abnormal in the monofilament, 60% abnormal in the biothesiometer, and 83% abnormal in the heat-washout method.
We found that eight patients had orthostatic hypotension measured by orthostatic blood pressure, and we found correlation between the heat-washout method and the orthostatic blood pressure result in nine patients (60%) assuming that lack of the veno-arteriolar reflex in one leg was an indication of autonomic neuropathy.
Discussion
In the present study we evaluated the use of the heat-washout method for identifying peripheral neuropathy by examining the veno-arteriolar reflex and compared the results with the most commonly used bedside methods to diagnose peripheral neuropathy in the fall assessment. We found impaired veno-arteriolar reflex in 93% of the elderly fall patients diagnosed with peripheral neuropathy, and found a relatively good correlation between impaired veno-arteriolar reflex and orthostatic hypotension.
Furthermore, in the six remaining patients with diverse result in the heat-washout method and the orthostatic blood pressure, we observed that the veno-arteriolar reflex was impaired without the orthostatic blood pressure was affected. This may indicate that an impaired veno-arteriolar reflex is present earlier than the orthostatic blood pressure is affected in peripheral neuropathy, but this needs to be studied in a larger follow up study.
We found impaired vibration perception in all fifteen patients (three patients had only abnormal vibration perception in one leg), when tested with the tuning fork. We found consistency between the result of the tuning fork and the biothesiometer in 63%, both tests evaluating vibrotactile perception. Furthermore, we only found consensus in 63% of the three simple methods to evaluate large fibre neuropathy. This concordance is similar to a cross-sectional study comparing the routine clinical tools for distal symmetric polyneuropathy, comprising the tuning fork and the monofilament with the biothesiometer and the skin biopsy36.
This discrepancy may reflect the concern that the biothesiometer, the monofilament, and the tuning fork are potentially challenged by variation in the clinical examination comprising testing technique, for instance disagreements about exact pressure applied and testing anatomic site selection, furthermore, varying interpretation of the findings, for instance, if loss of the vibrotactile perception may be a normal physical finding in the very old subjects or indicates peripheral neuropathy27,41. Moreover, cognitively impaired patients may have difficulties understand and respond verbally to the test, and thus indicating if the perception of the monofilament, the biothesiometer, or the tuning fork is perceived.
We found impaired veno-arteriolar reflex in fourteen of the fifteen elderly fall patients (93%) diagnosed with peripheral neuropathy at the Fall clinic indicating peripheral autonomic neuropathy26,42.
The heat-washout method is an objective, non-invasive test, which is easy to perform and without any discomfort for the patient. Furthermore, the method is age-independent and can be used without considering the patient’s cognitive or physical performance.
The heat-washout method examines the small, unmyelated C fibre in the peripheral autonomic nervous system, which may be associated with postural hypotension26,42. A previous study found that the veno-arteriolar reflex seems to be reduced in patients with distal peripheral neuropathy causing postural hypotension, when examined with the laser Doppler Flowmetry43.
Small fibre neuropathy can be difficult to identify, because the clinical signs of small fibre neuropathy are usually minimal44. The consequence can be disabling though, therefore, the use of a reliable, objective method to increase the sensitivity of the peripheral autonomic neuropathy diagnosis may be valuable. Furthermore, previous studies primarily concerning diabetic neuropathy have proposed that small fibre neuropathy might be the first sign of neuropathy, and therefore tests which predominantly assess the status of the small fibre may be valuable to establish preventive care16,18,45,46.
It is essential to consider that the monofilament, the biothesiometer, and the tuning fork evaluate the presence of large fibre sensory neuropathy, whereas the heat-washout method assess the small, unmyelated C fibre26. However, in many conditions, peripheral neuropathy is probably a mixture of small and large fibres neuropathy15. Consequently we could not identify a substantial association between the results of the heat-washout method and the results from the monofilament, the tuning fork, and the biothesiometer, but the result is consistent with previous studies combining the routine clinical tools5,34,36.
However, the clinical evaluation of peripheral neuropathy is challenged by depending on unavailable and time-consuming test as the nerve conduction study, or be dependent of tests that rely primarily on the subjects’ verbal response as the monofilament, the tuning fork, and the biothesiometer. Additionally, the most commonly used routine clinical tools for assessing peripheral neuropathy primarily assess the large fibre and may not be effective in detecting peripheral autonomic neuropathy8,47. Therefore, the heat-washout method may be a valuable supplement for assessing peripheral neuropathy, particularly in the elderly, fall patients, considering that peripheral autonomic neuropathy is an important element in the causal pathway to falls among the elderly48, and the test is independent of the patients cognitive status. Especially given that a decline in cognitive performance is associated with increased risk of falls, and many fall patients are cognitive impaired49,50.
This study indicates that the heat-washout method may be useful for assessing peripheral autonomic neuropathy in the elderly, but more studies of larger well-defined groups of elderly patients with and without peripheral neuropathy, as well as comparable studies with the heat-washout method and other methods testing the sympathetic response, for instance, the sudomotor axon reflex test, the cardiovagal and adrenergic autonomic testing, the Valsalva manoeuvre and the skin biopsy are recommendable.
This study has some limitations. Firstly, we included a relatively small number of patients, and we did not assess if the orthostatic hypotension could be due to other diseases or drugs.
Furthermore, in this study we did not apply any amnestic neurological symptoms or score system for evaluating neuropathy, for instance, the Diabetic Neuropathy Examination score system or the Diabetic Neuropathy Symptom score system, because the evidence are sparse, and the score systems are developed and tested on diabetics15. Furthermore, the selected cut-off value for the different tests may be debatable, and thus result in inaccurate evaluation, but the most common evaluations were used.
Additionally, the clinical history may be unreliable, and testing methods to examine peripheral sensory neuropathy such as the monofilament, the tuning fork, and the biothesiometer depend entirely on the patient’s statements6,8.
The most commonly used methods to assess peripheral neuropathy have primarily been made to evaluate diabetic neuropathy among relatively young subjects, therefore, more studies on the elderly fall patients is relevant, especially assessment of the peripheral autonomic dysfunction, since it can be subclinical, might precede large fibre neuropathy, and it is an important risk factor for falls and overall mortality16,18,19,27,28,44,45.
Conclusion
The prevalence of peripheral neuropathy is increasing with age, and associated with increased fall risk. The routine clinical tools to diagnose peripheral nerve dysfunction may be inaccurate and inapplicable to the elderly patients.
The aim of this study was to compare the heat-washout method with the three commonly used routine clinical tools, the monofilament, the tuning fork, and the biothesiometer in fifteen fall patients diagnosed with peripheral neuropathy. Furthermore, we compared the result of the heat-washout method with the results of the orthostatic blood pressure.
The result of the heat-washout method was consistent with the results of the biothesiometer in 50%, with the tuning fork in 73%, and with the monofilament in 70%. We only found consensus between the three routine clinical tests in 63%, although all tests evaluate peripheral large fibre neuropathy.
We found impaired veno-arteriolar reflex in 93% of the patients diagnosed with peripheral neuropathy, and found a relative good correlation between impaired veno-arteriolar reflex and orthostatic hypotension.
The heat-washout method may be a valuable supplement for examining peripheral neuropathy, especially in elderly patients, who might be cognitively impaired, given that the heat-washout method is an objective, non-invasive, age independent method without any discomfort for the patient. Furthermore, the method evaluate the peripheral small fibre nervous system, which may be the first indication of peripheral neuropathy, but difficult to identify with non-invasive methods.
We therefore conclude that the heat-washout method may be useful for assessing peripheral autonomic neuropathy in elderly patients.
Authors contribution
Le Gjerum examined the patients and drafted the manuscript and interpreted data. Mette Midttun revised the manuscript and interpreted the data.
Authors’ information
Le Gjerum, MD, Danish Dementia Research Centre, Rigshospitalet, University of Copenhagen, DK-2100 Copenhagen, Denmark.
Corresponding author: Mette Midttun, MD, MDSC, Department of Internal Medicine, Geriatric section, Copenhagen University Hospital, DK-2730 Herlev, Denmark.
Acknowledgements
The authors wish to thank the Fall clinic at Department of Internal Medicine, Geriatric Section, Copenhagen University Hospital, Herlev, Denmark.
References
- Herwaldt LA, Pottinger JM. Preventing Falls in the Elderly. Journal of the American Geriatrics Society. 2003; 51: 1175-1177.
- Sherrington C, Tiedemann A, Fairhall N, et al. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. New South Wales Public Health Bulletin. 2011; 22: 78-83.
- Steadman J, Donaldson N, Kalra L. A randomized controlled trial of an enhanced balance training program to improve mobility and reduce falls in elderly patients. Journal of the American Geriatrics Society. 2003; 51: 847-852.
- Youkhana S, Dean CM, Wolff M, et al. Yoga-based exercise improves balance and mobility in people aged 60 and over: A systematic review and meta-analysis. Age and Ageing. 2016; 45: 21-29.
- Callaghan B, Price R, Feldman E. Diagnostic and Therapeutic Advances: Distal Symmetric Polyneuropathy. JAMA Neurol. 2015; 314: 2172-2181.
- Richardson JK. Factors associated with falls in older patients with diffuse polyneuropathy. Journal of the American Geriatrics Society. 2002; 50: 1767-1773.
- Richardson JK, Thies SB, DeMott TK, et al. A comparison of gait characteristics between older women with and without peripheral neuropathy in standard and challenging environments. Journal of the American Geriatrics Society. 2004; 52: 1532-1537.
- de Mettelinge T, Calders P, Palmans T, et al. Vibration perception threshold in relation to postural control and fall risk assessment in elderly. Disability and rehabilitation. 2013; 35: 1712-7.
- Richardson J, Sandman D, Vela S. A focused exercise regimen improves clinical measures of balance in patients with peripheral neuropathy. Archives of physical medicine and rehabilitation. 2001; 82: 205-209.
- Richardson JK, Hurvitz E. A Peripheral neuropathy: a true risk factor for falls. The journals of gerontology. Series A Biological sciences and medical sciences. 1995; 50: M211-M215.
- Bonnet CT, Ray C. Peripheral neuropathy may not be the only fundamental reason explaining increased sway in diabetic individuals. Clinical Biomechanics. 2011; 26: 699-706.
- Tilling LM, Darawil K, Britton M. Falls as a complication of diabetes mellitus in older people. Journal of Diabetes and its Complications. 2006; 20: 158-162.
- Volpato S, Leveille SG, Blaum C, et al. Risk Factors for Falls in Older Disabled Women With Diabetes: The Women’s Health and Aging Study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2005; 60: 1539-1545.
- Resnick HE, Stansberry KB, Harris TB, et al. Diabetes, peripheral neuropathy, and old age disability. Muscle and Nerve. 2002; 25: 43-50.
- Williams D, Conn J, Talley N, et al. Reviewing the evidence base for the peripheral sensory examination. International Journal of Clinical Practice. 2014; 68: 756-760.
- Körei AE, Istenes I, Papanas N, et al. Small-Fiber Neuropathy: A Diabetic Microvascular Complication of Special Clinical, Diagnostic, and Prognostic Importance. Angiology. 2016; 67: 49-57.
- England JD, Asbury AK. Peripheral neuropathy. Lancet. 2004; 363: 2151-2161.
- Lacomis D. Small-fiber neuropathy. Muscle and Nerve. 2002; 26: 173-188.
- Biaggioni I. New developments in the management of neurogenic orthostatic hypotension. Current cardiology reports. 2014; 16: 542.
- Weiss A, Chagnac A, Beloosesky Y, et al. Orthostatic hypotension in the elderly: are the diagnostic criteria adequate. Journal of Human Hypertension. 2004; 18: 301-305.
- Vissing S, Secher N, Victor R. Mechanisms of cutaneous vasoconstriction during upright posture. Acta physiologica Scandinavica. 1997; 159: 131-8.
- Santiago S, Ferrer T, Espinosa ML. Neurophysiological studies of thin myelinated (A delta) and unmyelinated (C) fibers: Application to peripheral neuropathies. Neurophysiologie Clinique. 2000; 30: 27-42.
- Belcaro G, Nicolaides AN. The venoarteriolar response in diabetics. Angiology. 1991; 42: 827-835.
- Cacciatori V, Dellera A, Bellavere F, et al. Comparative assessment of peripheral sympathetic function by postural vasoconstriction arteriolar reflex and sympathetic skin response in NIDDM patients. American Journal of Medicine. 1997; 102: 365-370.
- Midttun M, Ahmadzay NF, Henriksen JH. Does comprilan bandage have any influence on peripheral perfusion in patients with oedema. Clinical Physiology and Functional Imaging. 2010; 30: 323-327.
- Midttun M, Snorgaard O. Heat-washout - an objective method for diagnosing neuropathy and atherosclerosis in diabetic patients. Clinical Physiology and Functional Imaging. 2013; 33: 302-306.
- Mold, JW, Vesely SK, Keyl BA et al. The prevalence, predictors, and consequences of peripheral sensory neuropathy in older patients. The Journal of the American Board of Family Practice/American Board of Family Practice. 2004; 17: 309-18.
- Richardson JK. The clinical identification of peripheral neuropathy among older persons. Archives of Physical Medicine and Rehabilitation. 2002; 83: 1553-1558.
- Amstrong D. The 10-g Monofilament. Diabetes Care. 2000; 23: 887.
- Phulpoto JA, Gurbakhshani KM, Shaikh A. Role of bedside methods in evaluation of diabetic peripheral neuropathy. Rawal Medical Journal. 2012; 37: 137-141.
- Kanji JN, Anglin RES, Hunt DL. Does This Patient With Diabetes Have Large-Fiber Peripheral Neuropathy. JAMA. 2010; 303: 1526-1532.
- Sundhedsstyrelsen. Faldpatienter I Den Kliniske Hverdag. 2006.
- Sundhedsstyrelsen. Diabetiske fodsår en teknologivurdering. Medicinsk Teknologivurdering. 2011; 13: 323.
- Dros J, Wewerinke A, Bindels PJ, et al. Accuracy of Monofi lament Testing to Diagnose Peripheral Neuropathy. Annals Of Family Medicine. 2009; 7: 555-558.
- WHO. ICD-10: International statistical classification of diseases and related health problems. 2016; 3.
- Pourhamidi K, Dahlin, LB, Englund E, et al. Evaluation of clinical tools and their diagnostic use in distal symmetric polyneuropathy. Primary Care Diabetes. 2014; 8: 77-84.
- O’Brien T, Karem J. An Initial Evaluation of a Proof-of-Concept 128-Hz Electronic Tuning Fork in the Detection of Peripheral Neuropathy. Journal of the American Podiatric Medical Association. 2014; 104: 134-140.
- Jones PK, Gibbons CH. Autonomic function testing: an important diagnostic test for patients with syncope. Practical Neurology. 2015; 15: 346-351.
- Kaufmann H. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multple system atrophy. Clin Auton Res. 1996; 6: 2.
- Midttun M, Sejrsen P, Colding Jorgensen M. Heat-washout: a new method for measuring cutaneous blood flow rate in areas with and without arteriovenous anastomoses. Clinical physiology Oxford, England. 1996; 16: 259-274.
- Maffei L, Premrou V1, Roldan P, et al. Vibration Perception Threshold in the Screening of Sensorimotor Distal Symmetric Polyneuropathy: The Need of More Accurate Age-Specific Reference Values. Journal of Diabetes Science and Technology. 2014; 8: 621-622.
- Kuritzky L, Espay AJ, Gelblum J, et al. Diagnosing and treating neurogenic orthostatic hypotension in primary care. Postgraduate medicine. 2015; 127: 702-15.
- Iwase M, Imoto H, Murata A, et al. Altered postural regulation of foot skin oxygenation and blood flow in patients with type 2 diabetes mellitus. Experimental and Clinical Endocrinology and Diabetes. 2007; 115: 444-447.
- Tobin K, Giuliani MJ, Lacomis D. Comparison of different modalities for detection of small fiber neuropathy. Clinical Neurophysiology. 1999; 110: 1909-1912.
- Kihara M, Mitsui M, Nishikawa S, et al. Comparison of electrophysiologic and autonomic tests in sensory diabetic neuropathy. Clinical Autonomic Research. 1998; 8: 213-220.
- Devigili G, Tugnoli V, Penza P, et al. The diagnostic criteria for small fibre neuropathy: From symptoms to neuropathology. Brain. 2008; 131: 1912-1925.
- Vinik AI, Freeman R, Erbas T. Diabetic Autonomic Neuropathy. Seminars in Neurology. 2003; 23.
- Quigley PA, Bulat T, Schulz B, et al. Exercise Interventions, Gait, and Balance in Older Subjects with Distal Symmetric Polyneuropathy. American Journal of Physical Medicine & Rehabilitation. 2014; 93: 1-16.
- Fischer BL, Gleason CE, Gangnon RE, et al. Declining Cognition and Falls: Role of Risky Performance of Everyday Mobility Activities. 2014; 94.
- Grobe S, Kakar RS2, Smith ML, et al. Impact of cognitive fatigue on gait and sway among older adults: A literature review. Preventive Medicine Reports. 2017; 6: 88-93.
