Commentary on the NeBoP score - a clinical prediction test for children with Lyme neuroborreliosis
Barbro H Skogman1*, Johanna Sjöwall2, Per-Eric Lindgren3
Headline
A new clinical prediction test has been developed for evaluation of children with Lyme neuroborreliosis in a European setting. Such a tool for decision-making about early antibiotic treatment has not earlier been presented and is suggested to be useful in a clinical setting.
Background
The diagnosis of Lyme neuroborreliosis in Europe is based on clinical symptoms and laboratory data, such as pleocytosis and anti-Borrelia antibodies in serum and CSF according to guidelines1. However, the decision to start antibiotic treatment on admission cannot be based on Borrelia serology since results are not available at the time of lumbar puncture. Therefore, an early prediction test would be useful in clinical practice. Previous studies have suggested different clinical prediction rules but patients have not been representative of all children with Lyme neuroborreliosis in Europe2-4. We can here present a study based on a large representative sample of children being evaluated for Lyme neuroborreliosis in a European Lyme endemic area.
Material and method
Clinical and laboratory data were collected retrospectively from a cohort of children being evaluated for Lyme neuroborreliosis in Southeast Sweden. A clinical neuroborreliosis prediction test, the NeBoP score, was designed to differentiate between a high and a low risk of having Lyme neuroborreliosis. It included variables such as acute facial nerve palsy (or other cranial nerve palsy), fever, fatigue, erythema migrans and/or lymphocytoma and pleocytosis in CSF (with total cell count ≥ 5 × 106/L with ≥ 90 % mononuclear cells) (Figure 1). A score of ≥ 3 points was considered as positive test. The NeBoP score was prospectively validated in another cohort of children being evaluated for Lyme neuroborreliosis in Central and Southeast Sweden (n=190) and controls with other specific diagnoses (n= 49).
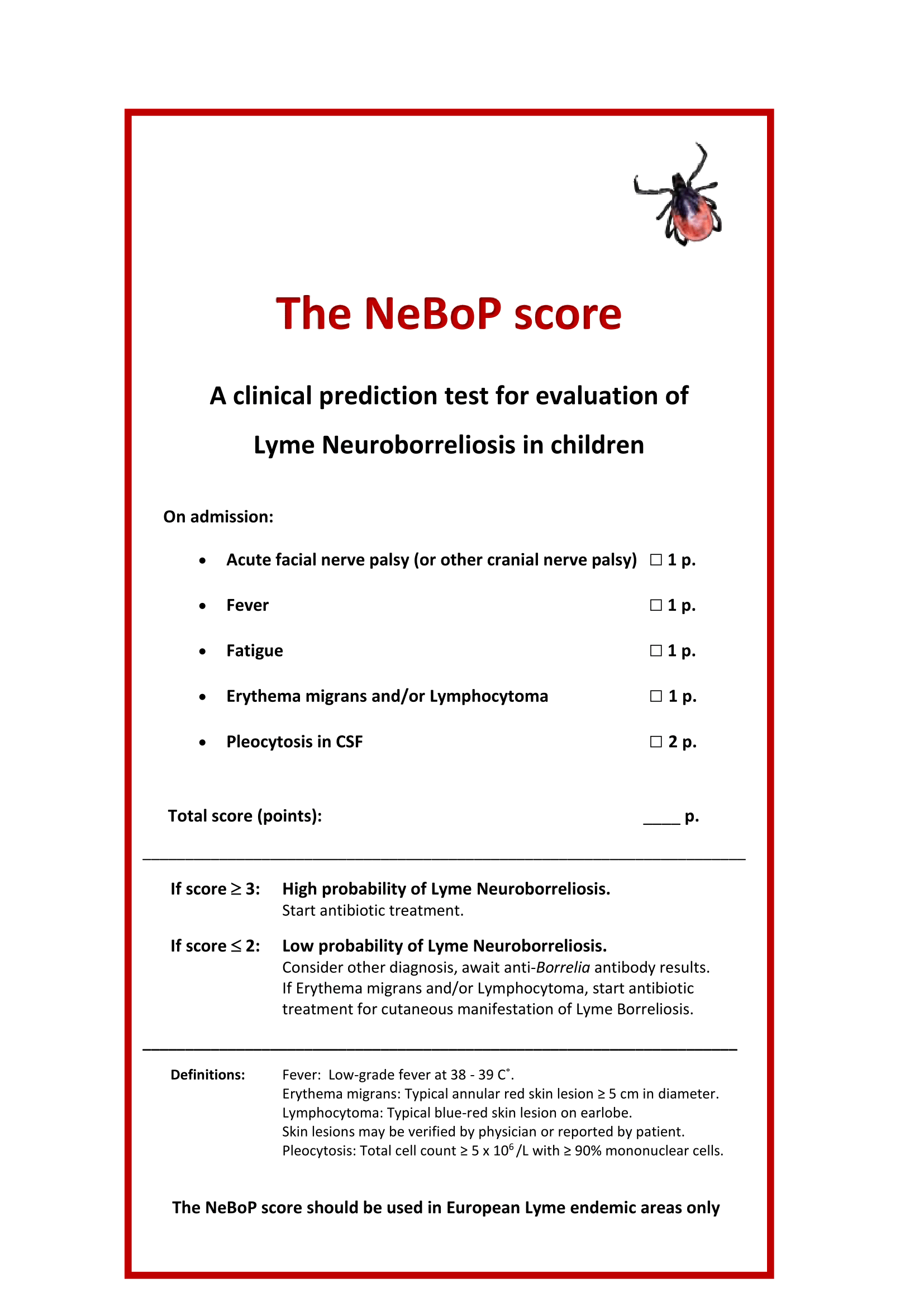
Figure 1: The NeBoP score
Results
The sensitivity of the NeBoP score was 90% (CI 95%; 82-99%) and the specificity was 90% (CI 95%; 85-96%). Thus, the diagnostic accuracy (i.e. how the test correctly discriminates patients from controls) was 90% and the area under the curve in a ROC analysis was 0.95. The positive predictive value (PPV) was 0.83 (CI 95%; 0.75 – 0.93) and the negative predictive value (NPV) was 0.95 (CI 95%; 0.90 – 0.99).
Discussion
Our results support that this clinical predictive test, the NeBoP score, could be useful for pediatricians in early assessment of children being evaluated for Lyme neuroborreliosis However, the NeBoP score cannot be recommended for Northern America due to differences in the clinical manifestations of Lyme neuroborreliosis,, the occurrence of different tick vectors and different Borrelia species between the two continents. We also believe, based a NPV of 0.95 for the NeBoP score, that the test will be helpful for the pediatrician to correctly refrain from unnecessary antibiotic treatment on admission and consider other differential diagnoses while waiting for anti-Borrelia antibody results. This aspect is, in our opinion, also important in order to prevent over usage of antibiotics. Furthermore, other CNS infections should be evaluated in parallel to LNB5.
Conclusion
The overall diagnostic performance of the NeBoP score is high (90%) and the test is suggested to be useful when evaluating children being evaluated for Lyme neuroborreliosis in European Lyme endemic areas.
Author’s comments
A clinical prediction test would be useful also for adult patients being evaluated for Lyme neuroborreliosis, but such a test has to our knowledge not yet been developed.
References
- Mygland A, Ljostad U, Fingerle V, Rupprecht T, Schmutzhard E, Steiner I. EFNS guidelines on the diagnosis and management of European Lyme neuroborreliosis. Eur J Neurol. 2010; 17(1):8-16, e11-14.
- Nigrovic LE, Thompson AD, Fine AM, Kimia A. Clinical predictors of Lyme disease among children with a peripheral facial palsy at an emergency department in a Lyme disease-endemic area. Pediatrics. 2008; 122(5):e1080-1085.
- Cohn KA, Thompson AD, Shah SS, Hines EM, Lyons TW, Welsh EJ, Nigrovic LE. Validation of a clinical prediction rule to distinguish Lyme meningitis from aseptic meningitis. Pediatrics. 2012; 129(1):e46-53.
- Tuerlinckx D, Bodart E, Jamart J, Glupczynski Y. Prediction of Lyme meningitis based on a logistic regression model using clinical and cerebrospinal fluid analysis: a European study. Pediatr Infect Dis J. 2009; 28(5):394-397.
- Henkel K, Eiffert H, Nau R and Spreer A: Infections in the differential diagnosis of Bell's palsy: a plea for performing CSF analysis. Infection. 2016; DOI 10.1007/s15010-016-0933-8