Contrast Induced Encephalopathy: Case Report and Review of The Literature
Sarah Kawtharani1, Elias Horanieh2, Bader Ali3, Mohammad Housheimy1, Houssein Darwish1*
1Department of Neurosurgery, American University of Beirut Medical Center, Beirut, Lebanon
2Department of Surgery, University of Balamand, Beirut, Lebanon
3Medical Student, University of Balamand, Beirut, Lebanon
Abstract
Background: Contrast Induced Encephalopathy is a known but rare complication of endovascular procedures. Patients show neurologic symptoms mimicking a stroke and include visual disturbances, motor or sensory deficits, headache, seizures, memory loss, confusion, aphasia, and coma. Irreversible neurological symptoms are rare and fatal encephalopathy is even more so.
Case Report: In this article we present a case of a 75-year-old female patient who showed neurological symptoms mimicking a stroke post cerebral Digital Subtraction Angiography that was done with Iohexol as a contrast agent, as a diagnostic work up to rule out a ruptured aneurysm. Further investigations showed no arterial spasms nor dissection. Symptoms reappeared after the second contrast administration but completely resolved after the administration of steroids and fluids.
Conclusion: Contrast Induced Encephalopathy should be further investigated with imaging to rule out other thromboembolic or hemorrhagic causes. Treatment via the administration of steroids and fluids have shown to be effective with complete remission of symptoms.
Introduction
Contrast induced encephalopathy (CIE) is a widely known yet infrequently documented complication of cerebral angiography and endovascular procedures. It is defined as an abrupt onset of mild to severe neurological deficits following the administration of intravascular contrast media5. CIE was first confirmed and reported in 1961 but was originally identified in 1956. However, it was not established as a definite diagnosis due to the absence of neuroimaging to rule out other potential causes17,18. CIE was seen in 0.06%, 0.3% to 1%, and 2.9% of patients undergoing coronary angiogram, vertebral angioplasty and cerebral aneurysm coiling, respectively7,10,15,16. The incidence can increase up to 4% after the use of hyperosmolar iodinated contrast material10. CIE patients may experience transient episodes of visual disturbances, motor or sensory deficits, headache, seizures, memory loss, confusion, aphasia, and coma12. The majority of patients fully recover within 48 to 72 hours of the procedure, with a minority improving after a few weeks. Irreversible neurological symptoms and even fatal encephalopathy were documented in previous case reports but are extremely rare10,14. Fatal CIE has been seen in about 8 cases reported in the literature so far8. A study by Chu et al. in 2020 showed that renal dysfunction (GFR <45), heart failure, prior stroke, and anticoagulant use are the most significant risk factors to develop CIE3.
In this article, we describe a patient who showed symptoms of contrast-induced encephalopathy mimicking a stroke after undergoing Digital Subtraction Angiography (DSA).
Case
We present a case of a 75-year-old female patient who is right-handed, known to have hypertension, dyslipidemia, and hypothyroidism who presented to the ER for severe excruciating headache of 5-hour duration that awakened her from sleep. The headache was described as a knife-like sensation over her head that radiated to her spine. Pain was 10/10 on severity scale. The pain had a positional component. It occurred mainly upon movement of her head or neck, coughing, and was associated with nausea and vomiting. Before the procedure, no motor or sensory deficits, cranial nerves intact, Glasgow Coma Scale (GCS) was 15, vital signs within normal limits, and creatinine level was <1mg/dl. CT brain showed moderate subarachnoid hemorrhage at the skull base, in the peri-mesencephalic area suspicious for ruptured aneurysm (Figure 1). CT-angiography (CTA) was done to investigate the possibility of a ruptured aneurysm but no aneurysm was identified and all the intracranial vasculature were patent. The patient was admitted to the Neurological ICU for observation and further assessment. Given the fact the patient had a negative CTA with the bleed involving the peri-mesencephalic cisterns, venous bleed was the suspected diagnosis. We elected to do DSA to confirm the diagnosis and to confirm the absence of any ruptured aneurysm that could be missed on CTA. DSA was done, the anterior and posterior circulation was visualized with no ruptured aneurysm seen which confirmed our initial diagnosis. The patient finished the procedure in good condition and left the angio-suite without neurological deficits; she was awake, moving all 4 extremities with full power, verbalizing and had intact peripheral lower extremity pulses. After arrival to the ICU by around 20 minutes, the patient showed signs of aphasia, right hemi-neglect with left homonymous hemianopia. The patient was rushed to DSA again which did not show any signs of vasospasm or dissection and all the intracranial vessels were patent. To note that the patient's exam improved on the way to the angio-suite, where she was verbalizing and had resolved hemineglect. We noticed that upon giving contrast during the second procedure, in the left common carotid artery, the patient showed the same symptoms again and improved after giving IV hydration and dexamethasone 16mg stress dose and was kept on 8mg q8h that was then tapered over 2 weeks. Her symptomatology is consistent with contrast induced encephalopathy that improved within 15-20 min from medical treatment with complete resolution in 45 min with normal blood flow in the anterior and posterior circulation without any vascular compromise as seen in Figures 2 and 3. Repeat CT scan 6 hours later did not show any increase in the previous bleed. The patient’s symptoms totally resolved after adequate hydration and steroid intake. The patient was in the ICU for 2 days post procedure, transferred to regular floor for 1 day, then discharge home on the 4th day.
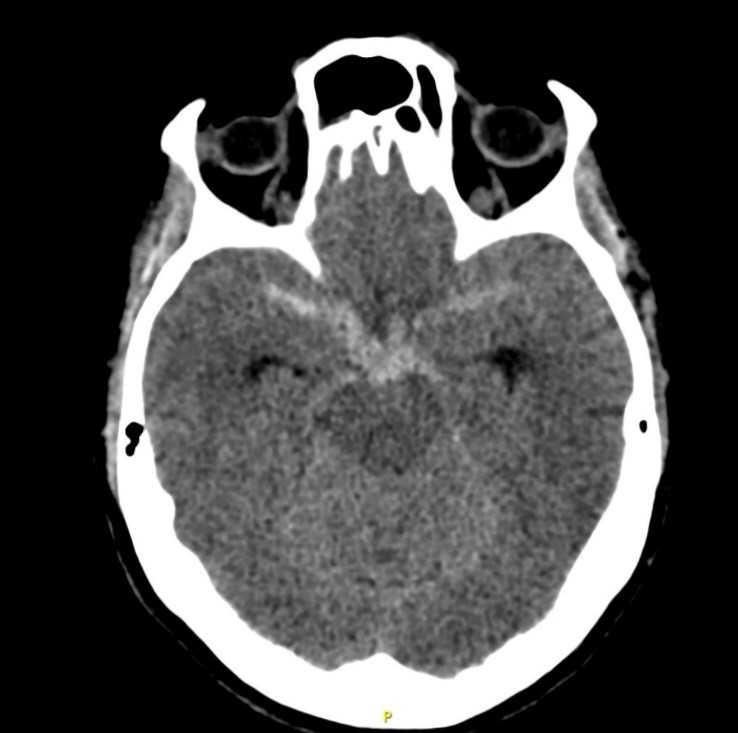
Figure 1: Brain CT without contrast, axial cut showing peri-mesencephalic subarachnoid hemorrhage
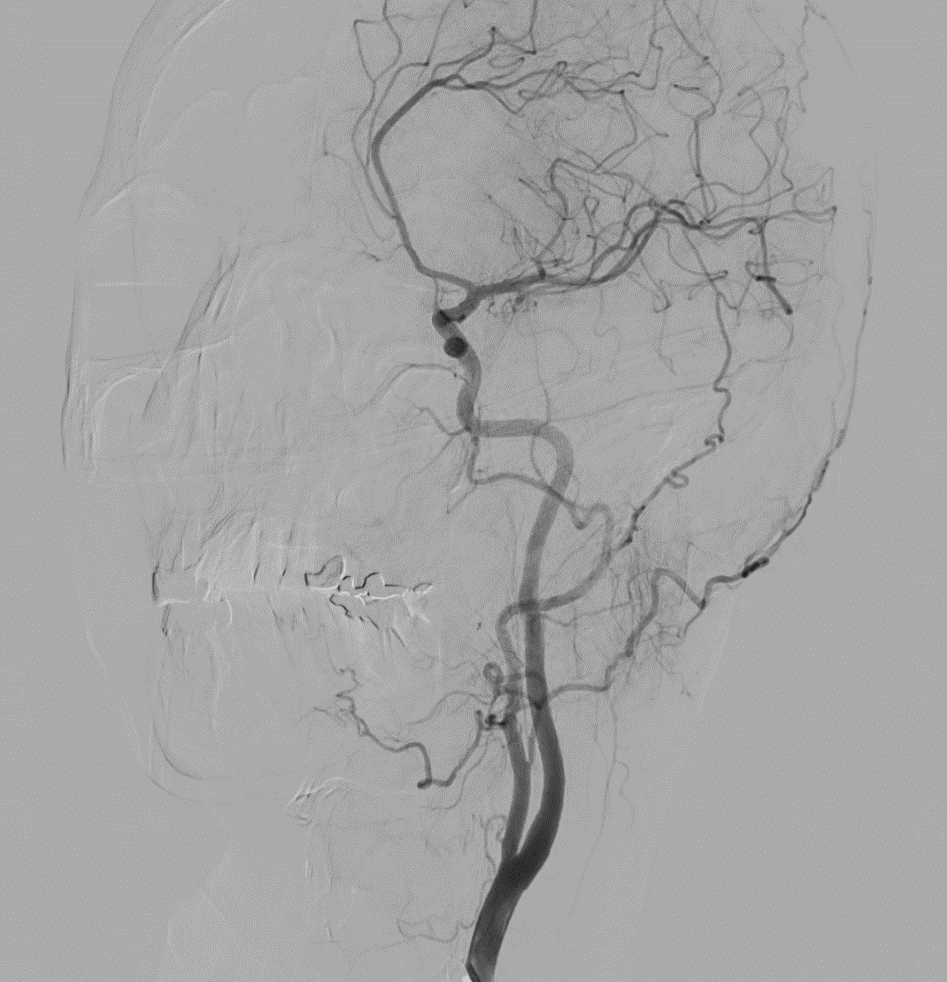
Figure 2: DSA imaging showing normal blood flow in the anterior circulation

Figure 3: DSA imaging showing normal blood flow in the posterior circulation
Discussion
Contrast Induced Encephalopathy is a rare complication due to the administration of intravascular contrast media during cerebral angiography and endovascular procedures with a prevalence of less than 5%3,5,15,21. According to a multicentric study done by Li et al., risk factors include injection of large doses, angiography of the posterior circulation, kidney disorders, diabetes, and hypertension1. Although, the pathophysiology of CIE is still not fully understood6, it has been theorized that the disruption in the blood brain barrier is the initial step in the development of this entity. This theory could explain the predominance of cortical blindness in most cases since the blood brain barrier is most permeable in the occipital region20. The use of hyperosmolar contrast agents is associated with most cases of CIE while non-ionic iso-osmolar agents were found to have neurological toxicity but less severe outcomes10. As predicted from the literature, our patient had visual disturbances, aphasia, and left hemineglect (Table 1). It is worthy to note that our patient received an injection of Iohexol (sold under the name of Omnipaque) which is a non-ionic, iodinated, iso-osmolar contrast agent.
In most cases, CIE mimics subarachnoid hemorrhage radiologically and a stroke clinically. In our patient, the stroke mimicking symptoms can be localized to the region supplied by the middle cerebral artery. Therefore, neuroimaging (CT or MRI) is essential as soon as the patient starts showing neurological symptoms during or after the procedure. The diagnosis of CIE can be confirmed by ruling out other thromboembolic or hemorrhagic events. CT scans show brain swelling due to vasogenic edema with sulcal effacement and increased density of the CSF10,11,22 while brain MRI can sometimes be negative since it shows normal or increased intensity in case of vasogenic edema. Once the diagnosis of CIE is made, treatment options can either be simple supportive therapy that includes hydrations and antiseizure medications or the administration of steroids. Both treatment modalities were offered in the literature (Table 1), and both have shown similar results of full recovery within hours or days. In our case, the patient received a combination of hydration and steroids with complete recovery.
Table 1: Literature review of contrast induced encephalopathy post endovascular procedures
|
Reference |
Age (years) /Sex (M/F) |
Endovascular procedure |
Symptoms post procedure |
Treatment |
Outcome |
|
Babalova et al.1 |
57/M |
Posterior cerebral artery angiography |
Bilateral vision loss, oculomotor dysfunction, right eye deviation, disorientation and somnolence, fever (38 degrees) |
Mannitol, antibiotics, antipyretics |
Full recovery within 6 days |
|
Vigano et al.20 |
56/F |
Cerebral angiography for SAH |
Global aphasia and right hemiplegia |
Dexamethasone and Sodium chloride |
Full recovery in 10 days |
|
Monforte et al.13 |
70/M |
Left carotid artery angiography |
Impaired consciousness, partial seizures |
Valproate |
Full recovery within 3 days |
|
Spina et al.19 |
52 patients Average 60 years/63% F |
Coronary angiography |
Global aphasia, weakness, seizures, oculomotor ophthalmoplegia, cortical blindness, confusion, agitation, amnesia |
Supportive care (37 patients) Thrombolysis with antiplatelets (3 patients) Anticonvulsants and steroids in others |
Full recovery within 48-72 hours |
|
Zhang et al.23 |
22/F |
Bronchial arteriography |
Blurred vision, headache, nausea, vomiting, limb fatigue |
Mannitol, glucocorticoid, nimodipine, hydration |
Fully recovery within 3 days |
|
Capasso et al.2 |
75/M |
Abdominal CT angiography
|
Left hemiplegia with disorientation |
- |
Fully recovered within 24 hours |
|
Dattani el al.4 |
76/M |
Coronary angiography |
Confused, aggressive, GCS 12, |
Hydration |
Fully recovered within 9 days |
|
Kamimura et al.9 |
70/F |
Diagnostic cerebral angiography |
Drowsiness, high blood pressure (201/101 mmHG), GCS 13, seizures, eye deviation |
Methylprednisone and levetiracetam |
Fully recovered within 24 hours |
Conclusion
Contrast-Induced Encephalopathy is common and should be considered in any patient showing signs of stroke after undergoing angiographic or endovascular procedures. However, radiological imaging should still be done to rule out other thromboembolic or hemorrhagic causes that could explain the clinical symptoms. Although CIE is mostly reversible, it can lead to permanent neurological deficits mostly being visual disturbances. The administration of steroids has shown to improve the neurologic symptoms with complete remission.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgement
All authors contributed equally to this manuscript. All authors approved the final draft.
References
- Babalova L, Ruzinak R, Ballova J, et al. Contrast-induced encephalopathy. Bratisl Lek Listy. 2021; 122(9): 618-620. doi: 10.4149/BLL_2021_098. PMID: 34463105.
- Capasso R, Caranci F, Conforti R, et al. Contrast-induced encephalopathy after abdominal CT examination. Acta Neurol Belg. 2021; 121(5): 1325-1326. doi: 10.1007/s13760-021-01690-6. PMID: 33914294.
- Chu YT, Lee KP, Chen CH, et al. Contrast-Induced Encephalopathy After Endovascular Thrombectomy for Acute Ischemic Stroke. Stroke. 2020; 51(12): 3756-3759. doi: 10.1161/STROKEAHA.120.031518. PMID: 33121385.
- Dattani A, Au L, Tay KH, et al. Contrast-Induced Encephalopathy following Coronary Angiography with No Radiological Features: A Case Report and Literature Review. Cardiology. 2018; 139(3): 197-201. doi: 10.1159/000486636. PMID: 29402812.
- Deb-Chatterji M, Schäfer L, Grzyska U, et al. Stroke-mimics: an acute brainstem syndrome after intravenous contrast medium application as a rare cause of contrast-induced neurotoxicity. Clin Neurol Neurosurg. 2018; 174: 244-246.
- García-Pérez D, Parra-Serrano J, Panero I, et al. Transient cortical blindness secondary to contrast-induced encephalopathy following diagnostic cerebral angiography: report of 2 cases. Acta Neurol Belg. 2021; 121: 585-589.
- Harada Y, Kairamkonda SR, Ilyas U, et al. Pearls & Oy-sters: Contrast induced encephalopathy following coronary angiography: A rare stroke mimic. Neurology. 2020.
- Junck L, Marshall WH. Fatal brain edema after contrast-agent overdose. AJNR: American Journal of Neuroradiology. 1986; 7(3): 522.
- Kamimura T, Nakamori M, Imamura E, et al. Low-dose Contrast-induced Encephalopathy During Diagnostic Cerebral Angiography. Intern Med. 2021; 60(4): 629-633. doi: 10.2169/internalmedicine.5139-20. PMID: 32999223; PMCID: PMC7946509.
- Leong S, Fanning NF. Persistent neurological deficit from iodinated contrast encephalopathy following intracranial aneurysm coiling: a case report and review of the literature. Interventional Neuroradiology. 2012; 18(1): 33-41.
- Liu M, Jiang H, Li X, et al. Case report and literature review on low-osmolar, non-ionic iodine-based contrast-induced encephalopathy. Clinical Interventions in Aging. 2020: 2277-2289.
- Merchut MP, Richie B. Transient visuospatial disorder from angiographic contrast. Arch Neurol. 2002; 59(5): 851-854.
- Monforte M, Marca GD, Lozupone E. Contrast-induced Encephalopathy. Neurol India. 2020; 68(3): 718-719. doi: 10.4103/0028-3886.288986. PMID: 32643703.
- Nakao K, Joshi G, Hirose Y, et al. Rare cases of contrast-induced encephalopathies. Asian Journal of Neurosurgery. 2020; 15(03): 786-793.
- Niimi Y, Kupersmith MJ, Ahmad S, et al. Cortical blindness, transient and otherwise, associated with detachable coil embolization of intracranial aneurysms. Am J Neuroradiol. 2008; 29(3): 603-607.
- Potsi S, Chourmouzi D, Moumtzouoglou A, et al. Transient contrast encephalopathy after carotid angiography mimicking diffuse subarachnoid haemorrhage. Neurological Sciences. 2012; 33: 445-448.
- Quintas-Neves M, Araújo JM, Xavier SA, et al. Contrast-induced neurotoxicity related to neurological endovascular procedures: a systematic review. Acta Neurol Belg. 2020; 120: 1419-1424.
- Silverman SM, Bergman PS, Bender MB. The dynamics of transient cerebral blindness: report of nine episodes following vertebral angiography. Arch Neurol. 1961; 4(3): 333-348.
- Spina R, Simon N, Markus R, et al. Contrast-induced encephalopathy following cardiac catheterization. Catheter Cardiovasc Interv. 2017; 90(2): 257-268. doi: 10.1002/ccd.26871. PMID: 27896904.
- Vigano' M, Mantero V, Basilico P, et al. Contrast-induced encephalopathy mimicking total anterior circulation stroke: a case report and review of the literature. Neurological Sciences. 2021; 42(3): 1145-1150.
- Wishart DL. Complications in vertebral angiography as compared to non-vertebral cerebral angiography in 447 studies. Am J Roentgenol Radium Ther Nucl Med. 1971; 113(3): 527-37. doi: 10.2214/ajr.113.3.527. PMID: 5127714.
- Yu J, Dangas G. New insights into the risk factors of contrast-induced encephalopathy. Journal of Endovascular Therapy. 2011; 18(4): 545-546.
- Zhang F, Du X, Liu K. Contrast-induced encephalopathy following bronchial arteriography and endovascular procedure. Acta Neurol Belg. 2023; 123(2): 717-719. doi: 10.1007/s13760-022-02034-8. PMID: 35859227.
